Many security, policing, and military environments expose workers to chronic pressure. Security personnel must juggle competing demands under time constraints, working out how best to deploy scarce resources (time, skills, and equipment) to achieve optimal outcomes. Their lives and those of civilians are often at stake, threatened by unpredictable adversaries of uncertain capability and ambition. And then, sometimes, unexpected events occur that escalate and intensify this pressure such as the 2001 al-Qaeda attacks in New York or the Taliban’s swift takeover of Afghanistan in 2021.
Although not a security threat in the traditional sense, the early stages of the COVID-19 pandemic is a vivid example of a highly stressful and unexpected event. As enormous pressure was placed on healthcare systems around the world, frontline workers were quickly identified as being at increased risk of extreme stress and trauma exposure.
The psychological impact of novel, uncertain and traumatic events can be extraordinarily difficult to manage. Such situations often require a rapid response, whilst acute pressure piles on top of chronic pressures, in the glare of intense public scrutiny. But existing skills and previous training may be insufficient to respond to these new events.
Surge personnel – often inexperienced and under-trained – may need to be assimilated into existing teams. Standard operating procedures may prove ineffective and contingency plans may not be robust or even be non-existent. In these circumstances, personnel are forced to cope as best they can until effective plans can be implemented, sometimes for weeks at a time, often in the face of extraordinary human suffering, trauma, and death. How do workers cope with such novel, uncertain, dynamic, traumatic, and life-threatening sources of stress? How can their organisations best support them? And how can existing behavioural science research help in the face of acute pressures?
Personnel are forced to cope as best they can until effective plans can be implemented, sometimes for weeks at a time, often in the face of extraordinary human suffering, trauma, and death.
In this article, we describe some of the processes we followed and the lessons we learned. We discuss how these lessons can be applied to the work of security practitioners facing similarly demanding situations in the future.
Rapid response
Early in 2020 we were contacted by those coordinating the NHS’s COVID-19 response to develop a ‘Just-in-Time’ training and education curriculum to support frontline workers. The aim was to share the most up-to-date evidence and best practice related to ensuring the resilience, performance, and psychosocial health of frontline staff. Those coordinating the pandemic response quickly realised that it would force healthcare workers to operate in an entirely unfamiliar context. This was particularly the case for support staff being drafted in to fill gaps in healthcare provision and/or to provide relief to those key workers that were having to self-isolate after contracting the virus or symptoms.
Speed was critical to meeting these requirements. When they contacted us prior to the first national lockdown in March 2020, the NHS response team estimated they had approximately two weeks before a surge in hospitalised cases. This two-week window was an opportunity to establish ways of working that would contribute to resilient function, optimise performance and protect staff from mental ill-health in the weeks and months ahead.
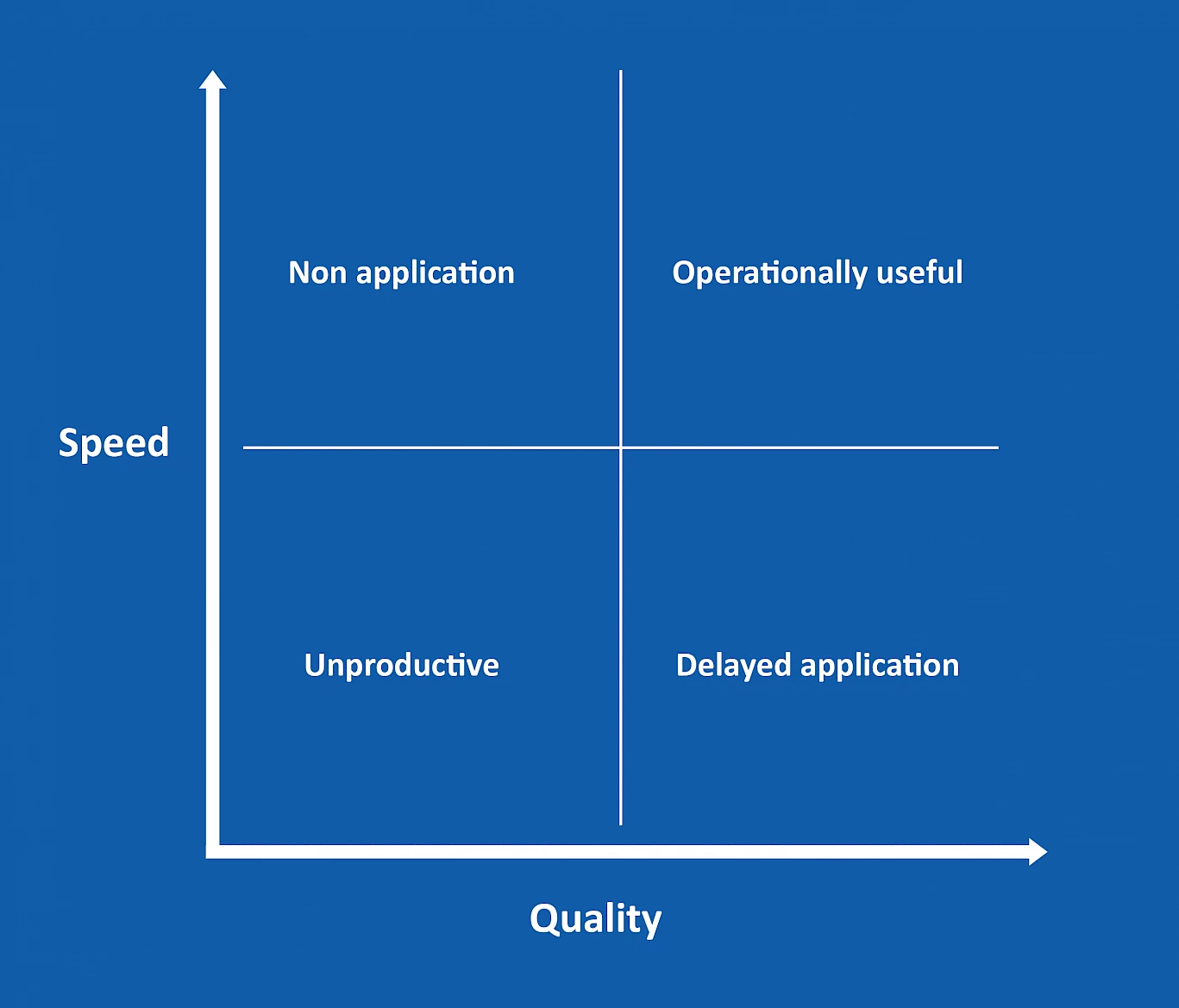
The message was clear: quality materials needed to be produced quickly if they were to be helpful and make a meaningful contribution. This demanded a balance between expediency and quality (Figure 1). Poor quality materials produced quickly were likely to be ignored by frontline workers (‘non application’) or risked giving harmful advice. Materials rigorously but slowly produced risked being applied at a late stage (‘delayed application’) and not meeting potential users' needs. We needed to work at pace but put in place assurance processes that helped us to ensure quality and to produce work that was operationally useful.
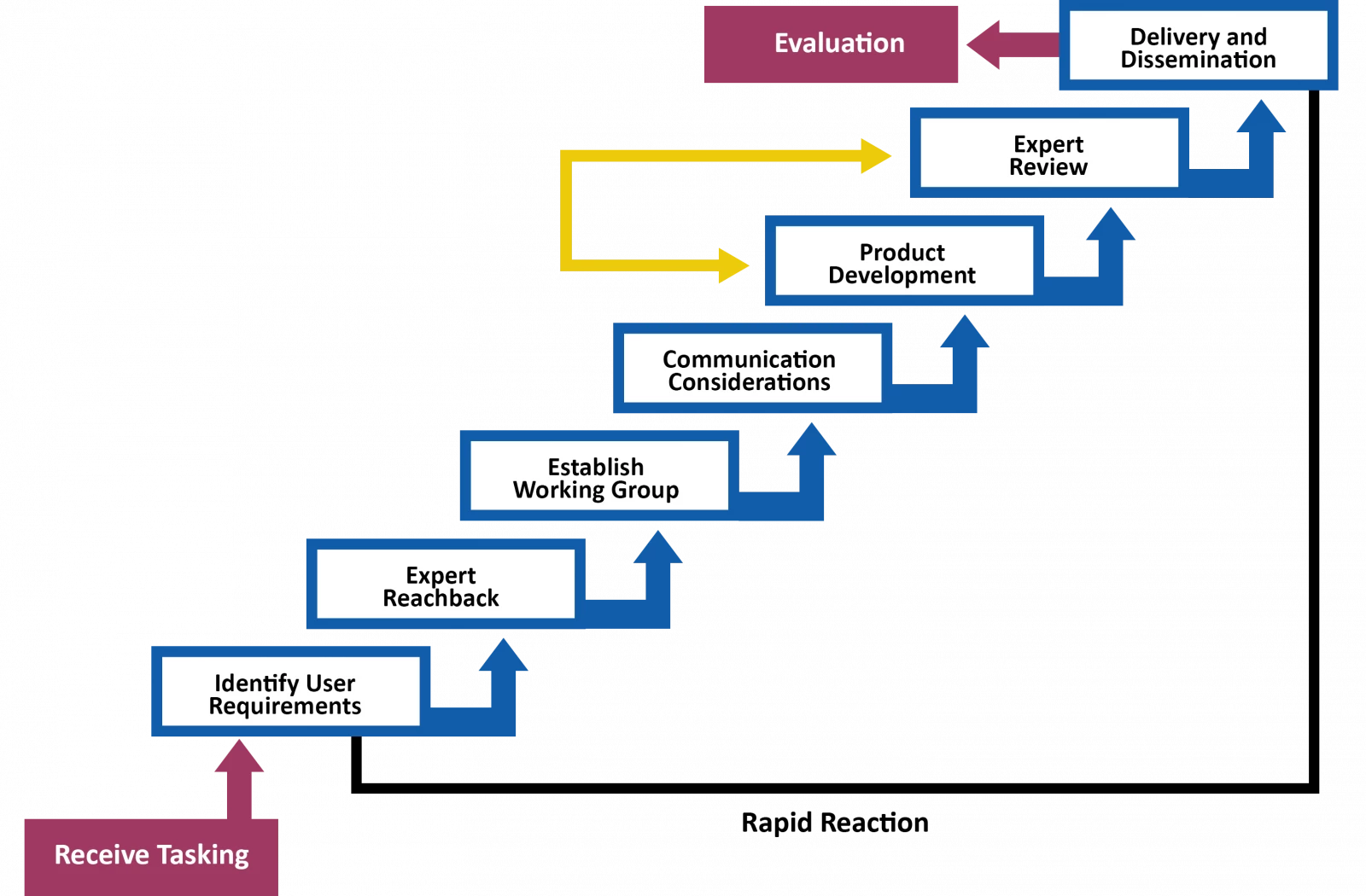
Our approach is presented in a rapid reaction model in Figure 2. We started by working with the NHS response team to identify their specific user requirements to ensure that what we produced was of genuine value to frontline workers. To ensure quality, we reached out to an expert consortium of academics and practitioners to establish an informal working group. Members of this group both wrote material and provided peer review of our and each other’s work. This was an essential step, providing a layer of quality control that gave credibility to our work. Through their invaluable hard work and expertise, peer review of material happened at pace, generally within 24 hours.
The early stages of the COVID-19 pandemic have much in common with novel, unexpected security events, and we believe that the lessons for frontline personnel are very similar.
Our outputs focused on how to engender resilient function at individual, group and organisational levels. We produced a series of evidence-based briefing notes that were directly informed by the requirements of end users. These covered topics including PTSD, moral injury, managing extreme stressors, understanding resilience, motivation, leadership, performance debriefing, readiness to work, decision making, team dynamics, fear of failure, isolation, and organisational culture. We worked with the NHS team to identify what communication and products would be most helpful. The requirement was for a series of briefs, that set out a clear rationale for the relevance of the subject, offering practical recommendations to complement rather than replace existing knowledge.
The design support was invaluable to ensure the briefing notes were clear and engaging. Notes were produced in both printable form and uploaded to a website (www.supporttheworkers.org) and we placed no restrictions on sharing. The notes were quickly shared throughout the UK (with the NHS and others involved in responding, such as military and security) and internationally (with the World Health Organisation and Johnson and Johnson Institute).
Amid a fast-moving operational response, we found it tricky to carry out a formal evaluation of the impact of our work. Our approach was to gather immediate feedback from the NHS team that tasked us on how the materials were being received at the frontline, which provided an opportunity to adjust and iterate our approach when developing additional resources. The feedback was gratifying, for example: “a collaboration of immense value and rigour in keeping us all grounded in best practice but without slowing our response ability down.”
Lessons for security
We draw two key lessons from this activity. First, it is essential that materials produced during crises, such as during the response to a terrorist incident or fast-changing diplomatic situation, are both shaped by end-user needs and designed for that audience. Resisting the urge to spring into immediate action and instead taking time to speak to a range of end users will help ensure materials produced are relevant and fit for purpose – as long as such consultation can be done quickly.
Second, we have shown it is possible to produce a response that is both rapid and of high quality. Confirming response timeframes is crucial for effectively communicating and managing expectations of both end users and experts. Much can be done in a very short space of time if people are committed and conscious of the time pressure. In our case, two weeks was enough to access available expertise and evidence and to put in place robust and rapid peer review processes.
In terms of the acute stressors placed on frontline personnel, the early stages of the COVID-19 pandemic have much in common with novel, unexpected security events, and we believe that the lessons for frontline personnel are very similar. Indeed, some of the evidence we drew on for our briefs was derived in security settings. Our briefs may therefore be of value to security personnel with minimal editing. However, novel circumstances may arise in future that demand additional or different research briefing notes and we suggest that the rapid response approach we adopted for COVID-19, and in particular focusing on end user requirements and maximising the opportunity for evidence-based practice, may provide useful direction for security practitioners responding to significant events in their work.
Read more
- Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., … & Wang, J. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry, 7, e15-e16
- Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ, 368
- Knutson, A., Park, N. D., Smith, D., Tracy, K., Reed, D. J., & Olsen, S. L. (2015). Just-in-time training: a novel approach to quality improvement education. Neonatal Network, 34, 6-9
- Leach, J. (2016). Psychological factors in exceptional, extreme and torturous environments. Extreme physiology & medicine, 5, 7.
- Maguire, M., & Bevan, N. (2002, August). User requirements analysis. In IFIP World Computer Congress, TC 13 (pp. 133-148). Springer, Boston, MA.
- Smith, N., & Barrett, E. C. (2019). Psychology, extreme environments, and counter-terrorism operations. Behavioral sciences of terrorism and political aggression, 11, 48-72
- Williamson, V., Murphy, D., & Greenberg, N. (2020). COVID-19 and experiences of moral injury in front-line key workers. Occupational Medicine
- Wu, H. L., Huang, J., Zhang, C. J., He, Z., & Ming, W. K. (2020). Facemask shortage and the novel coronavirus disease (COVID-19) outbreak: Reflections on public health measures. EClinicalMedicine, 100329
Copyright Information
As part of CREST’s commitment to open access research, this text is available under a Creative Commons BY-NC-SA 4.0 licence. Please refer to our Copyright page for full details.
IMAGE CREDITS: Copyright ©2024 R. Stevens / CREST (CC BY-SA 4.0)